Testicular Cancer Treatment in Singapore
Effective
Supportive

of Experience


Care & Support
Early detection of testicular cancer can make all the difference.
What Is Testicular Cancer?
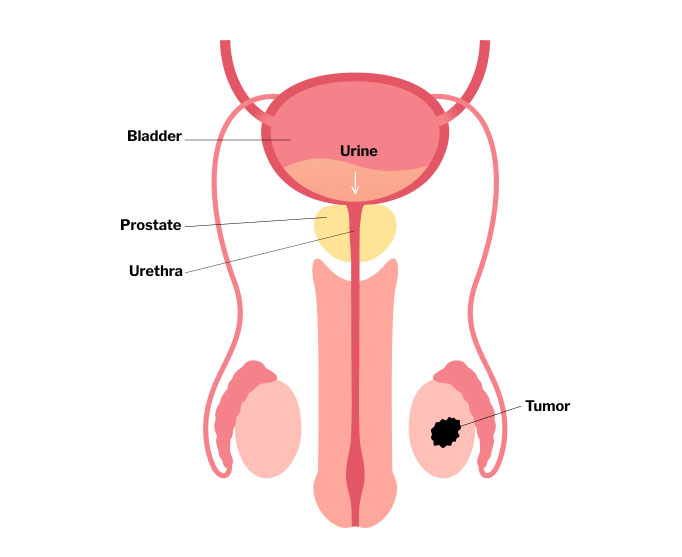
Testicular cancer occurs when abnormal cells grow uncontrollably in one or both testicles. The testicles (or testes) are part of the male reproductive system and are located in the scrotum. They are responsible for producing sperm and testosterone.
The majority of testicular cancers are germ cell tumours, which are further divided into:
- Seminomas – Slower-growing and more sensitive to radiation and chemotherapy
- Non-seminomas – These tend to grow more quickly but also respond well to chemotherapy
What are the Symptoms of Testicular Cancer?
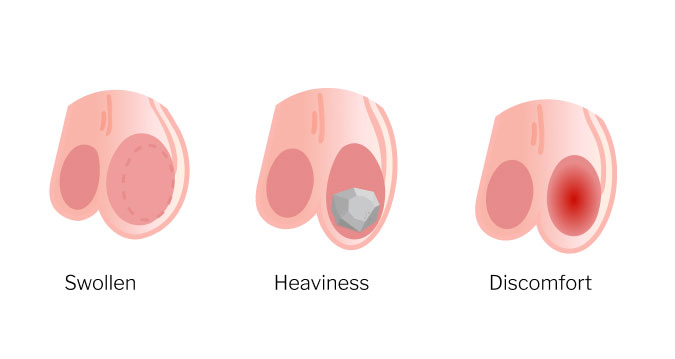
Early-stage testicular cancer is often painless. The most common presenting sign is a lump or swelling in the testicle. Other symptoms may include:
- A painless lump or enlargement in either testicle
- A feeling of heaviness in the scrotum
- Dull ache in the lower abdomen or groin
- Sudden collection of fluid in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Enlargement or tenderness of breast tissue (less common)
These symptoms are not always due to cancer—but any persistent change in the testicle should be promptly assessed by a urologist.
Concerned about a testicular lump?
Call 6518 3622 to schedule a consultation with our testicular cancer specialist.

Who is at Risk of Testicular Cancer?
Risk factors for testicular cancer include:
- Undescended testicle (cryptorchidism)
- Family history of testicular cancer
- Previous history of testicular cancer
- Abnormal testicular development (e.g., Klinefelter syndrome)
- Age – most common in men aged 15 to 40
Regular testicular self-examinations are encouraged for those at higher risk of developing testicular cancer.
How Is Testicular Cancer Diagnosed?
If testicular cancer is suspected, the diagnostic process typically includes:

Physical examination of the testicles

Scrotal ultrasound to evaluate any lumps or swelling

Blood tests for tumour markers

CT scan of the abdomen and chest to check for spread
In most cases, a firm or suspicious mass may require removal of the affected testicle for both diagnosis and treatment.
Staging of Testicular Cancer
After diagnosis, testicular cancer is staged to determine how far it has spread:
STAGE I
Confined to the testicle
STAGE II
Spread to lymph nodes in the abdomen
STAGE III
Spread to distant organs such as the lungs
What are the Treatments for Testicular Cancer in Singapore?
Testicular cancer treatment depends on the type and stage of the tumour. Common treatments include:
Radical Inguinal Orchiectomy
Surgical removal of the affected testicle is usually the first line of treatment for both seminomas and non-seminomas. The procedure is performed through an incision in the groin, rather than the scrotum, to avoid spreading cancer cells. This surgery not only treats the primary tumour but also helps confirm the diagnosis through laboratory analysis.
Surveillance
For some early-stage (Stage I) testicular cancers, particularly seminomas, surgery may be followed by active surveillance instead of immediate additional treatment. This approach involves regular follow-up appointments, including blood tests (tumour markers), imaging scans, and physical exams, to detect any signs of recurrence. It’s often recommended when the risk of recurrence is low.
Chemotherapy
Chemotherapy is often used in cases of non-seminomas or advanced-stage seminomas, where the cancer may have spread beyond the testicle. It involves the use of anti-cancer drugs to kill cancer cells throughout the body. Chemotherapy may be given after surgery (adjuvant therapy) to reduce the risk of recurrence, or as the primary treatment for metastatic disease. Most patients respond very well to standard regimens.
Radiation Therapy
Radiation is mainly used for seminomas, which are particularly sensitive to it. The therapy is directed at retroperitoneal lymph nodes (located in the back of the abdomen) to destroy any microscopic cancer cells that may have spread. It’s generally not used for non-seminomas, which are less responsive to radiation.
Retroperitoneal Lymph Node Dissection (RPLND)
In some cases, especially for non-seminomas or when lymph nodes remain enlarged after chemotherapy, RPLND may be performed. This surgery involves the removal of lymph nodes in the back of the abdomen (retroperitoneum) to ensure no cancer remains or to more accurately stage the disease. It is a specialised procedure done by trained urologic surgeons.

Fertility Considerations and Follow-Up
Since testicular cancer often affects young men, fertility preservation is an important consideration. Patients may be advised to store sperm before undergoing treatment that may affect fertility, such as chemotherapy or RPLND.
Long-term follow-up includes:
- Regular tumour marker testing
- Imaging studies
- Physical examination
Most recurrences occur within the first 2 years, so close monitoring during this period is essential.
When to See a Urologist for Suspected Testicular Cancer
You should seek medical evaluation if you:
- Notice a lump, swelling, or firmness in the testicle
- Experience persistent scrotal discomfort or heaviness
- Have a history of undescended testicle or prior testicular cancer
- Are unsure about self-examination findings

Our Testicular Cancer Specialist
Dr Tan Teck Wei
MBBS (S’pore), DFD (CAW), MRCS (Edin),
MMed (Surgery), FAMS (Urology)
Dr Tan Teck Wei is a Senior Consultant Urologist and former Director of Genitourinary Oncology at Tan Tock Seng Hospital. Skilled in the management of testicular cancer, Dr Tan strives to provide empathetic and effective care with the patient’s best interests in mind. He is fellowship-trained in open, laparoscopic and robotic urologic surgery; and has held numerous leadership and academic positions. Dr Tan understands the distress faced by patients and their families, and is committed to providing care that is not only medically sound but also supportive, personalised, and attuned to each patient’s circumstances.
FAQs on Testicular Cancer
A painless lump or swelling in one testicle is the most common sign. Some men may also feel a dull ache or heaviness in the scrotum.
It most commonly affects younger men between ages 15 and 40.
Diagnosis typically involves a physical exam, ultrasound, and blood tests for tumour markers.
Yes. Testicular cancer has a high cure rate, even if it has spread, especially when treated promptly.
Fertility can be affected, particularly with chemotherapy. Sperm banking is often recommended before treatment begins.
For enquiries on your condition or appointment booking, please fill in the enquiry form and we will be in touch with you soon. Your health and well-being are our top priorities, and we look forward to assisting you on your medical journey.